Achilles Tendinitis (or Achilles Tendonitis) is a common foot disorder that affects athletes and physically active people. This condition of the foot and ankle involves the Achilles tendon, the largest tendon connecting calf muscles to the heel bone.
The main cause of tendon pain is Achilles Tendinitis. An overly stressed tendon becomes irritated and inflamed, which often results in pain and swelling. If left untreated, it can lead to Achilles tendon rupture.
Achilles tendinitis treatment includes physical therapy, supportive shoes and rest. Surgery may be necessary if the symptoms don’t go away.
What is Achilles Tendinitis?
Tendinitis is the irritation or inflammation of the tendon. Inflammation is your body’s reaction to disease or injury. It often results in severe pain and swelling of the affected area, in this case, the Achilles tendon.
If you have tendinitis in your Achilles tendon, it’s crucial to seek treatment right away. Otherwise, it may lead to a long-term, chronic problem that makes walking difficult.
Types of Achilles Tendinitis
Insertional Achilles Tendinitis
Insertional Achilles tendinitis affects the lower part of the heel. It is the area where the tendon inserts or connects to the heel bone.
This type of Achilles tendinitis affects anyone, even those who are not physically active. However, it is more common in people like long-distance runners who put a lot of stress on the Achilles tendon.
Noninsertional Achilles Tendinitis
Affecting younger and more active people, non insertional Achilles tendinitis is characterised by the breaking down of fibres in the middle part of the tendon, which often swell and thicken.
What are the symptoms of Achilles tendinitis?
Achilles tendinitis symptoms affects the lower leg and above the heel. You might notice:
Leg weakness.
Ankle and heel pain that worsens with physical activity.
Swelling or thickening around the Achilles tendon.
Either stiffness or tenderness in the tendon.
Limited range of motion every time you flex your foot.
The skin on the heel is warm to the touch.
You may notice severe aches and pains:
After a day of exercising or after physical activity.
After you go uphill or as you climb stairs.
You may have torn or ruptured your Achilles tendon if you experience a sudden “pop” in your heel or the back of your calf. If this happens, you should see your podiatrist as soon as possible to have your foot and ankle examined and treated.
What Causes Achilles Tendinitis?
Typically, Achilles Tendinitis is usually caused by overuse injury, and is the result of an overly stressed Achilles tendon. It happens when you push your body too much too soon. Since it’s difficult to avoid using this tendon, your body doesn’t have time to heal it.
What is an Achilles Tendon?
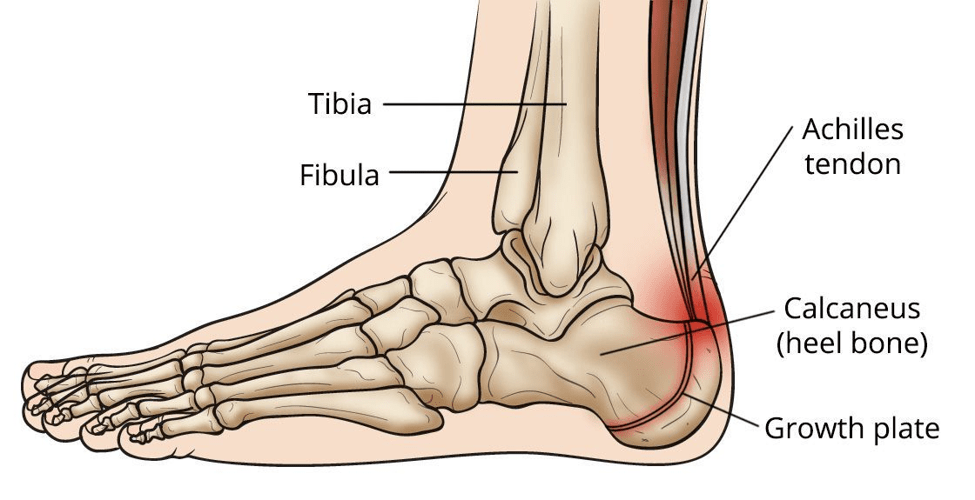 The Achilles tendon is located in the back of your heel. Your Achilles tendon works with your calf muscle and heel bone to raise your heel off the ground. It’s a tendon that helps you walk, run and jump.
The Achilles tendon is located in the back of your heel. Your Achilles tendon works with your calf muscle and heel bone to raise your heel off the ground. It’s a tendon that helps you walk, run and jump.
Named after the half-god from Greek mythology, the Achilles tendon is the largest tendon in the body. It connects your heel bone to your calf muscles.
Tendons are fibrous tissues that connect bones to muscles. They are made of long and tough collagen and elastin fibres.
What are the causes of Achilles tendon pain?
Achilles Tendinitis: Inflammation or irritation of the Achilles tendon.
Achilles Tendinosis: The breaking down of the Achilles tendon as a result of untreated tendinitis.
Achilles Tendon Rupture: A break or tear in the tendon.
Achilles Tendinopathy
Achilles tendinopathy is a longstanding injury resulting from tendon overuse. It is a painful syndrome affecting the Achilles tendon. Treatment includes physical therapy, non-steroidal anti-inflammatory drugs (NSAIDs) and rest.
Whilst Achilles tendinopathy is more common in younger people, professional and weekend athletes, it is also a common overuse injury in non-athletic people.
 There are 3 levels of severity in Achilles tendinopathy. These are:
There are 3 levels of severity in Achilles tendinopathy. These are:
Mild. Pain during an activity or shortly after.
Moderate. Swelling of the tendons and, in some cases, formation of hard lumps or nodules.
Severe. Pain is associated with weight-bearing activities, which often leads to tendon rupture.
Common causes of Achilles tendinopathy include:
Overuse injury
Arthritis
Foot problems
Ill-fitting footwear
Overweight and obesity
Diagnosis and Treatment for Achilles tendinopathy are similar to Achilles tendonitis.
Who is at risk for Achilles tendon Injuries?
Those who are at risk of Achilles tendon injuries are people who:
Run and dance frequently.
Play sports that involve stops and starts.
 Have jobs that overstress their feet and ankles.
Have jobs that overstress their feet and ankles.
Engage in sports less regularly, which leaves their bodies less used to the stress.
Moreover, your unique body shape, structure (anatomy) and function may also put you at risk of Achilles tendon disorders. Other factors can lead to Achilles Tendinitis if you have:
Sudden Intensity Increase of Exercise Activity
For instance, you’re not allowing your body to adjust when adding more distance to your daily running program.
Tight Calf Muscles
Suddenly starting an aggressive workout with tight calf muscles can put tremendous stress on your Achilles tendon.
Heel Bone Spur
Generally, the Achilles tendon is attached to the heel bone. A heel spur is an extra bone or calcification that grows from within the tendon near the heel. It can rub against the tendon and cause pain. The medical term for this condition is calcified achilles tendon.

Heel Pain or plantar fasciitis concept. Hand on foot as suffer from inflammation feet problem of Sever’s Disease or calcaneal apophysitis.
Overpronation
This happens when your foot rolls inward or your heel hits the ground first as you walk.
Flat Arches or Flat Fleet
How is Achilles tendinitis diagnosed?
 Your podiatrist will ask about your recent activity and symptoms. After you discuss your concerns and describe your symptoms, they will evaluate your foot and ankle.
Your podiatrist will ask about your recent activity and symptoms. After you discuss your concerns and describe your symptoms, they will evaluate your foot and ankle.
The podiatrist will look for signs of tendinitis or tendon rupture and examine your range of motion. Then he will also look for other signs such as:
Swelling at the lower calf or at the back of the heel
Enlarged or thickened Achilles tendon
Bone spurs at the tendon’s lower part (insertional Achilles tendinitis)
Pain in the tendon’s middle part (noninsertional tendinitis)
Tests to Diagnose Achilles Tendinitis
Your podiatrist can perform an Achilles tendinitis diagnosis based on the physical examination and discussing your pain with you. If required the podiatrist will order imaging like X-rays, diagnostic ultrasound or an MRI. In some cases imaging exams can guide treatment by reporting details of the tendon structure and health.
Imaging tests may include:
Magnetic Resonance Imaging (MRI)
Whilst, MRI is not necessary for Achilles tendinitis diagnosis, it can be helpful for planning surgery. An MRI scan can show the severity of tendon damage. If your Achilles tendinitis treatment requires surgery, your podiatric surgeon will perform a type of surgery based on the amount of tendon damage.
X-ray
An X-ray test can show clear images of your bones. It can show if the lower part of your Achilles tendon has calcified or hardened (calcified Achilles insertion). Similarly, X-rays can show calcification in the middle portion of the tendon (severe non insertional Achilles tendinitis).
Ultrasound
Sonography (Ultrasound) is an excellent way to evaluate your Achilles tendon. Your podiatrist may provide a diagnostic ultrasound in the office during your consultation. Some of its advantages are:
Cost
Availability
Ease of Contralateral comparison and
Ability to show images during joint motion
Achilles Tendonitis Treatment
Your podiatrist may recommend non-surgical treatment first. If you already had the symptoms of Achilles Tendonitis for a few months, the pain can take too long to get better.
Non-Surgical Achilles Tendonitis Treatment
The RICE Method
Rest. The first step to reducing pain on the Achilles tendon is to decrease or even stop doing high-impact exercises such as running, long jumps, burpees or jumping rope.
Instead, switch to low-impact activities such as swimming, elliptical exercise or biking. Cross-training activities and other low-impact options put less stress on the Achilles tendon whilst allowing you to stay active.
Ice. Putting ice on your inflamed or irritated tendon helps with pain relief and should be done as needed throughout the day. Do this for 20 minutes and must be stopped as soon as your skin becomes numb.
Compression: Put pressure on the tendon using an athletic wrap or surgical tape to compress the inflamed tendon. Another option is tying an article of clothing around the problem area. Make sure to wrap or tie just enough to keep the tendon from too much swelling whilst allowing proper blood flow.
Elevation: Raise your foot, making sure it is above chest level. This way, blood returns to your heart and reduces swelling. An easy way to do this is by lying down and putting your foot on a raised surface or a pillow.
Supportive Shoes, Orthotics and Shoe Inserts
 Certain shoes and orthotic devices can help reduce pain from insertional Achilles tendinitis. Supportive shoes and heel lifts help reduce irritation and strain on the tendon.
Certain shoes and orthotic devices can help reduce pain from insertional Achilles tendinitis. Supportive shoes and heel lifts help reduce irritation and strain on the tendon.
For severe pain, short-term use of a walking boot may be necessary. This method allows the tendon to rest before therapy begins. Note that long-term use of walking boots can weaken your calf muscles.
Non-Steroidal Anti-Inflammatory Drugs (NSAIDs)
Ibuprofen and Naproxen are anti-inflammatory drugs that help reduce pain and swelling of the Achilles tendon. However, they don’t address the thickening of degenerated tendons. You should avoid taking NSAIDs for more than a month without consulting your podiatric surgeon.
 Steroid Injections
Steroid Injections
Another effective medication for treating Achilles tendonitis is steroids. It is one of the most powerful anti-inflammatory drugs on the market. When your podiatric surgeon administered a steroid injection to your Achilles tendon they may require that you use a Moonboot. Steroid injection when administered in this manner will provide excellent and long-standing relief of pain.
Physical Therapy
Physical therapy is a proven non-surgical method for Achilles tendonitis treatment. It is known to work better for non insertional tendinitis cases.
This non-surgical treatment involves massage, stretching and strengthening exercises. There’s also a running re-education program to regain your strength and help you feel better.
Exercise
A good exercise routine (such as calf stretches) puts less stress on the Achilles tendon and help strengthen calf muscles. There are also certain exercises under the Eccentric Strengthening Protocol. However, the strengthening exercises can cause discomfort or damage to the Achilles tendon and so it requires the supervision of a physical therapist.
Extracorporeal Shockwave Therapy (ESWT)
EWST is a non-invasive Achilles tendonitis treatment with minimal risks involved. Shockwave therapy is often the preferred procedure before steroid injections or surgery is considered.
The ESWT procedure involves using high-energy shockwave impulses that stimulate a damaged tendon’s healing process. The treatment is usually administered once a week for 3 weeks. Tendon healing then occurs over 6 weeks. ESWT is an excellent treatment for Achilles tendon pain.
Surgical Achilles Tendonitis Treatment
Surgery for treating Achilles tendonitis is only considered if there is no improvement of pain after 3- 6 months of non-invasive treatment. Your podiatric foot and ankle surgeon can explain the best surgical options based on your activity level, injury, preferences and age. A specific type of surgery will depend on the location and severity of the damage on the tendon.
Gastrocnemius Recession
Since tight calf muscles overly stress the Achilles tendon, this type of surgery solves this problem by lengthening the gastrocnemius or calf muscles. Gastrocnemius recession is helpful for people still having difficulty flexing their feet despite stretching consistently.
Débridement and Repair
The goal of this type of surgery is to remove a tendon’s damaged part, provided that the damage is less than 50%. After the removal of the unhealthy portion, the remaining tendon tissues are repaired using stitches called sutures.
Débridement with Transfer of the Tendon
This operation is for an Achilles tendon with a damage of more than 50%, which means the remaining portion no longer has the strength to function properly. A tendon transfer is the best option to prevent the remaining portion from rupturing with activity.
Achilles Tendinitis? Contact Adelaide Foot and Ankle
If you think you have Achilles tendinitis, you should consult your foot and ankle doctor immediately. Initially, it is vital to diagnose your foot problem and determine its severity. Contact us today. We provide comprehensive care through accurate and timely diagnosis of your foot problem.







