Key Takeaways on Heel Spur
- The plantar fascia is a thick band found in the foot that stretches from the heel bone and connects to the ball of the foot (metatarsal heads), giving it its bowstring appearance.
- The recurring mechanical strain to the area leads to ossification or bony deposit build-up.
- Various studies show that being older predisposes a person to develop heel spurs due to the thinning of the fat pads on the soles of the feet.
- Whilst it is often assumed that heel pain is always caused by heel spurs, it is not the culprit for all kinds of pain felt in the heel.
- A heel spur is caused by long-term stress to the structures and may have developed as a response to them (especially to plantar fasciitis).
The heel is a frequent area that generates complaints of pain and discomfort. This is not surprising as the feet carry a considerable load—the rest of the body (not to mention additional weight outside of the body)—and bears a lot of impact, especially in high-impact activities.
Whilst there are several causes of heel pain—from traumatic, neurologic, and arthritic causes—most heel pain originates from mechanical sources. Of these, one of the most common causes is a heel spur. But what exactly is it?
This article shall discuss what a heel spur is, its causes, and its symptoms. It shall also discuss the risk factors that predispose a person to have it, how doctors diagnose it in a person and the different management or treatment that can be done.
What is a Heel Spur?

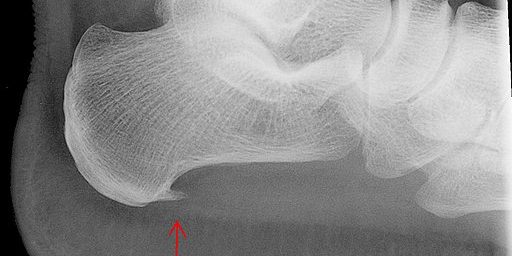
A calcaneal spur or enthesophyte, but more commonly known as a heel spur, is a pointed outgrowth under the heel bone (calcaneus bone) caused by bony deposit build-up.
A heel spur can either happen by itself or occur as part of a systemic inflammatory condition such as gout, Reiter’s syndrome, and Rheumatoid Arthritis.
Types of Heel Spurs
The American College of Foot and Ankle Surgeons (ACFAS) classifies plantar fasciosis, heel spurs, and plantar fasciitis under plantar heel pain.
On the other hand, a heel spur has two general types: one could be found along the bottom of the heel (plantar heel spur), and the other is located at the back of the heel (posterior or dorsal heel spur).
– Heel spurs found at the back of the heel are usually associated with an inflamed Achilles tendon. This often comes with tenderness and sharp pain when pushing off the heel from the floor when walking.
– Heel spurs at the back of the heel are often associated with plantar fasciitis or the inflammation of the plantar fascia. The plantar fascia is a thick band found in the foot that stretches from the heel bone and connects to the ball of the foot (metatarsal heads), giving it its bowstring appearance.
There are two types of plantar heel spurs:
Type A heel spur: the heel spur is above the insertion of the fascia
Type B heel spur: the heel spur extends forward from the heel bone towards the fascia
The length of type A heel spur is longer than that of type B heel spur. However, people with type B spurs report more significant pain than those with type A.
Heel spurs can also be classified into three distinct types:
Type 1: does not present with symptoms, large in size
Type 2: large in size and causes significant pain because the heel spur has become a weight-bearing point
Type 3: spur is irregular and jagged and presents with a little amount of proliferation
Is Heel Spur Common?
There is an 11-21% prevalence in the young to middle adulthood groups across different ethnicities. However, it was reported to occur more (55%) in people aged 62 and above.
To add, the same report found that it is more common to women than men.
Causes of Heel Spurs
Bone spurs are commonly caused by repeated inflammation and trauma at the area where the tendon of muscles and fascia attaches to the heel bone. It is also caused by repetitive stress and traction to the small muscles of the foot and the plantar fascia.
The recurring stress on the area leads to ossification or calcium deposit build-up. The resulting spur can extend up to half an inch and extends towards the arch of the foot over the course of months.
The repeated inflammation in this area happens due to any of the following:
– Repeated muscle strains
– Stretching of the plantar fascia
– Repetitive tearing of the membrane covering the heel bone
Occupations and activities that entail a great deal of standing or walking and require repetitive use and stress on the foot may develop heel spurs.
On the other hand, one study has found that heel spurs develop as the body’s adaptive response to mechanical stressors to prevent heel bone fractures.
Risk Factors

– Age. Various studies show that being older predisposes a person to develop heel spurs due to the thinning of the fat pads on the soles of the feet. To add, ligaments tend to ossify as a typical process of ageing. One study reported that 98% of heel spurs occur in people aged 40 and above, whilst another said that it occurs 55% in people aged 62 and above.
– Weight (46%). People who are overweight place much more pressure on the arch of the foot when walking. This may lead to injury and tearing of soft tissues in their foot.
– Gender. Especially in the younger population, women are more likely to have heel spurs than men. Some studies associate this with the altered foot biomechanics caused by wearing high heels.
– Foot Position. People whose feet are more rolled in (pronated foot) are more likely to develop heel spurs (62%). Also, 81% of people who complain of painful heel spurs are found radiographically to have pronated feet.
– Plantar Fasciitis. Heel spurs often occur with plantar fasciitis(67%).
– Arthritides. Heel spurs commonly occur in people with rheumatoid arthritis (RA), ankylosing spondylitis, osteoarthritis (OA), and psoriatic arthritis.
– Arch Structure. People who have either flat feet or high arches are prone to developing spurs.
– Activity Conditions. Jogging, running and jumping on hard surfaces, doing activities barefoot for prolonged periods, being active in certain sports, and doing regular physical activities in short bursts put stress on the foot’s soft tissue structures and may lead to developing heel spurs.
– Shoes worn. Wearing shoes that are ill-fitting or worn out makes them too loose. These shoes offer little support on the foot’s arches. In the same way, other shoes are too soft or lack the needed support for the arches of the foot.
Related post: What Can a Podiatrist Do for Plantar Fasciits?
Symptoms of Heel Spurs
Whilst it is often assumed that heel pain is always caused by heel spurs, it is not the culprit for all kinds of pain felt in the heel. Heel pain can also be caused by arthritis, trauma, nerve pain, and impingement of structures.
In many cases, a person has heel spurs but presents with no symptoms. In fact, most people only incidentally discover they have a heel spur when they have X- rays of their foot for a different purpose.
Also, most symptoms of spurs are symptoms of plantar fasciitis since they often occur together. Below are telltale signs that a person likely has heel spurs:
– Sharp pain felt at the sole at the initiation of weight-bearing, such as upon waking up or coming from a period of rest
– Consistent dull ache or presence of arch pain
– Pain when the heel, the arch of the feet, and the area in between is palpated
– Visible bone-like protrusion under the heel, which can be palpated
– Warmth, tenderness, and swelling in the affected area
It has to be noted, however, that heel spurs themselves do not usually cause pain, rather it is the irritation and inflammation of the structures around the heel that are painful. A heel spur is caused by long-term stress to the structures and may have developed as a response to them (especially to plantar fasciitis).
Diagnosis of Heel Spurs
Since the symptoms of plantar heel pain are well-known, its diagnosis is pretty straightforward. The podiatrist will do a thorough history which may include knowing about:
– the intensity and time(s) of day when the pain is felt
– the type of activities (both work and leisure) the person is engaging in, including exercises
– any history of trauma
– the shoes the person is using
– presence of sensory disturbances such as pins and needles (to exclude a neurologic cause of the heel pain)
– checking of other risk factors
After the podiatrist has reviewed the client’s health information, he will perform an exhaustive physical examination, which includes:
– checking the range of motion available in the foot and ankle with an emphasis on the available upward movement (dorsiflexion) of the foot
– palpating of the plantar fascia and the heel
– Increase in pain during weight-bearing
– Presence of skin tears on the foot
– checking for alterations in sensation
– observing for changes in muscle size (atrophy) or presence of swelling
– assessing the alignment of the foot
– doing a gait assessment
After the evaluation, the podiatrist may l recommend radiographic imaging. The presence of heel spurs on the radiographic image will confirm the diagnosis.
Suppose a person presents with symptoms typically associated with heel spurs but lacks X-ray imaging as evidence. In that case, the doctor may give a diagnosis of a “heel spur syndrome.”
Treatment for Heel Spurs

ACFAS provides three treatment options for heel pain following this timeline:
Tier 1: six weeks
Tier 2: six months
Tier 3: six months
Initial Treatment Options
The first line of management includes:
- Resting the structures
- Preventing any action that causes heel pain
- padding and strapping of the foot
- recommendation of orthotic insoles
- taking of oral anti-inflammatory medications (such as ibuprofen and naproxen) may reduce pain
- localised corticosteroid injection to help the person manage the pain.
Aside from these, a podiatrist may recommend the person to do specific management by themselves. These include:
– Regular stretching of the structures
– Doing light stretching exercises
– Choosing appropriate footwear
– Weight loss (in the case of patients with high BMI or those who are obese)
– Avoiding walking barefoot
– Icing the affected part
– Buying supports that are available over-the-counter such as heel cups, shoe inserts, and arch supports
– Limiting participation in extended high-impact activities
Second Tier of Treatment Options
If these treatment options work, the patient is to continue with the management until the symptoms resolve. If these do not resolve, the patient moves forward to the second tier of treatment options. The patient will continue with the treatments mentioned above and add a few more, which include:
– Use of orthotic devices (either prefabricated or custom-made)
– Wearing night splints that maintain the ankle in a certain position that stretches the calf muscles and ligaments as well as the plantar fascia
– Repeat corticosteroid injection
– Botox injection
– Immobilisation to offload the foot during activity via a cast or using a short-leg walking boot
– Physiotherapy programme
Third Tier of Treatment Options
If improvement is noted, both tier 1 and 2 treatment options are continued until the symptoms resolve. If they don’t resolve, the patient must continue with the first two tiers and proceed to the third tier where surgery may be recommended.
The third tier involves surgery directed at the fascia. Heel spurs are usually not surgically removed. In fact, removing a heel spur was not noted to contribute to the success of the outcome of surgical treatments.
A less invasive surgical alternative is extracorporeal shock wave therapy (ESWT). However, some heel pain is caused by other factors such as nerve entrapment. In these cases, other methods should be done in combination with surgery.
How Can You Prevent Heel Spurs?

Whilst heel spurs are pretty common, there are some things that a person can do to prevent yourself from developing heel spurs:
– Wearing shoes that fit well and are appropriate according to the activity
– Limit the use of high-heeled shoes
– Do proper warm-up and stretching
– Do proper pacing when doing activities
– Lose a few pounds if you are overweight
– Use shoe inserts, heel pads, and arch supports that protect the heel and arch
– When doing work that requires repetitive motion or stress on the foot, make a timetable with rests in between, when possible
– If you have incurred previous heel injuries, exercise due diligence in the activities and tasks that you do
– Limit participation in certain activities that would predispose the feet to incur injury
– Avoid walking or doing activities barefoot
– Be cautious when running or jumping or jogging on rough and hard surfaces
FAQs
Q: Do heel spurs go away?
A: No. They don’t usually cause problems. However, you can opt for surgical removal.
Q: How do you heal a heel spur?
A: You don’t target the heel spur per se but you manage the inflamed structures like the plantar fascia and tendons of foot muscles.
Q: What is plantar fasciitis?
A: Plantar fasciitis is the inflammation of the plantar fascia. It is a common cause of heel pain.
Q: What does a heel spur feel like?
A: Often, you will not feel anything. However, there may be a dull ache or a sharp pain depending on soft tissue damage.
Q: Does heel spur cause heel pain?
A: In itself, it does not cause pain. The inflammation and damage of soft tissue or tissues around the heel spur cause pain.
Q: What can I do to reduce pain caused by heel spurs and plantar fasciitis?
A: Pain may be reduced by taking anti-inflammatories. If symptoms do not resolve, seek medical advice
What is the Outlook for Heel Spurs?
Heel spurs have a positive outlook. The presence of bony deposits is usually not problematic. Treatment and management are directed toward managing pain and other symptoms such as inflammation and swelling.
In Summary
A spur is a bony protrusion that is one of the many causes of heel pain in relatively healthy and active individuals. Heel spurs have several causes and risk factors.
The good thing is heel spurs are pretty easy to diagnose and treat. Whilst some heel spurs cause a lot of pain, there’s no need to worry if you have heel spurs.
Not only are they manageable, but heel spurs have a very positive outlook as long as a person receives proper management and guidance from doctors and other related healthcare professionals.
Unsure if your heel pain is caused by heel spurs? Book an appointment with us, and we’ll conduct a thorough assessment of your foot so you get back on your feet in no time!
(xray image credit: Wikimedia)